GENERAL PAYOR SERVICEs
Details for select Service Offerings – CLAIMS EXPERIENCE & TREND ANALYTICS
» Summarize detailed healthcare claims data into homogenous service categories
» Calculate various metrics such as utilization rates, PMPM costs, provider discounts, actuarial value, medical loss ratio, and risk score.
» The reporting interface gives the user the ability to mass produce reports for various time periods, lines of business, market segments, healthcare providers, and clinical condition categories.
» Build custom tools to understand trend information on a total dollar, utilization, cost per service and per member per month basis, Allows multiple years of data to be presented on an annual, quarterly, monthly, or rolling 12-month basis. As part of the claims experience review, we help our clients understand drivers of medical and pharmacy claims trends:
- Utilization and member mix
- Unit cost, DRG mix, hospital mix, high and low outliers, fee schedule changes
- Traditional brand and generic drugs, specialty brand and generic drug trends, therapeutic class, top 25 drugs by sub classification
Claims Experience Review
Trend Analytics & Tools
Monthly Financial Close Support - IBNR Modeling and Revenue Performance
Year End Appointed Actuary
Rate Filings
Rate Manual Development
Pro Forma Development
Custom Dashboards
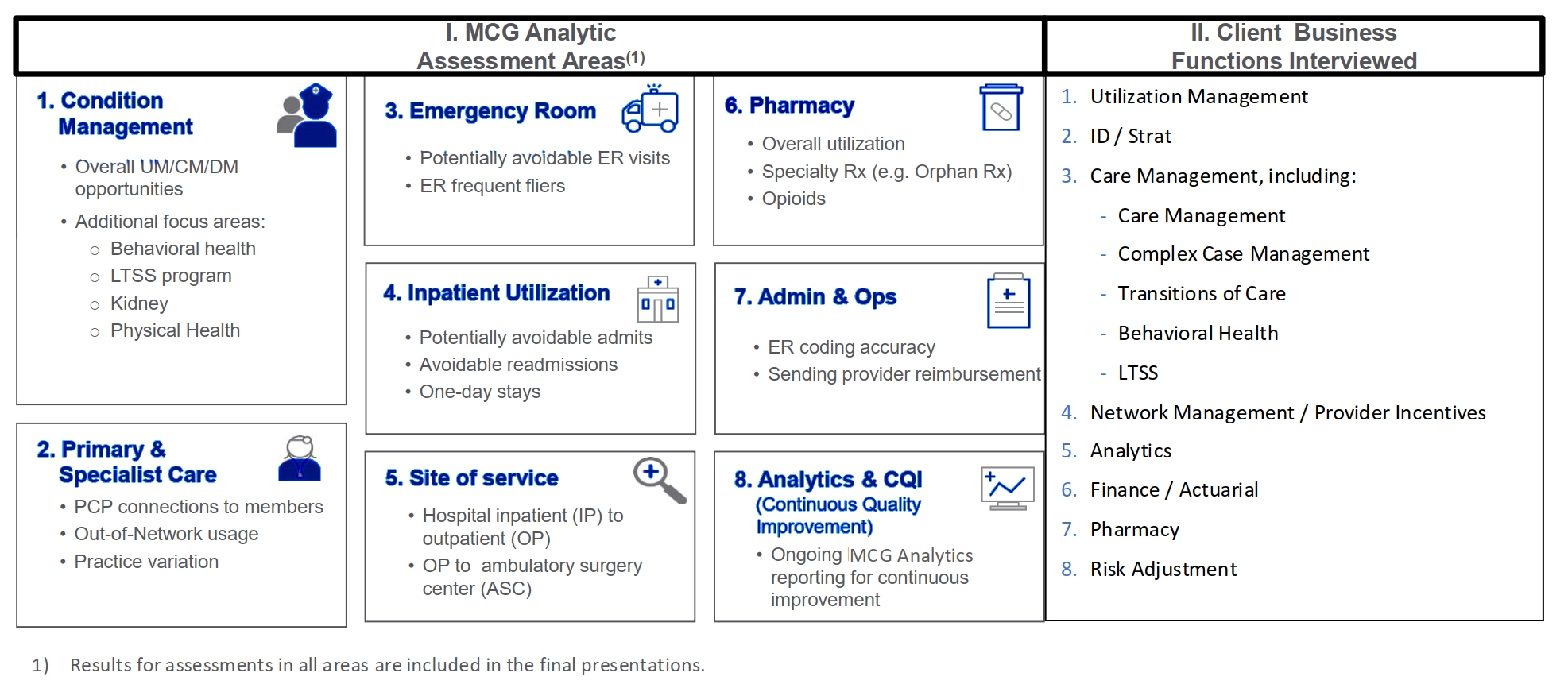
Risk Adjustment Accuracy – Chronic Conditions Gap